The Early detection in cases of familial breast cancer predisposition: What is appropriate and beneficial for the individual seeking advice?
DOI:
https://doi.org/10.59667/sjoranm.v2i1.13Keywords:
breast cancer, high risk, intensified surveillance, genetic testing, psychological aspects of patient management, participatory decision-makingAbstract
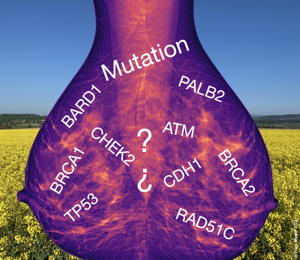
A "high-risk situation" is present when the lifetime risk of developing breast cancer is ≥ 30%. Currently, the most accurate risk assessment is provided by the Tyrer-Cuzick model. This takes into account several factors including the presence of certain risk genes, age, family history of breast and ovarian cancer, as well as mammographic breast density. In addition to BRCA1 and BRCA2 several other risk genes are known that can be tested using gene panels. However specific familial risk constellations are prerequisites for indicating a genetic test. Prior to conducting a genetic test comprehensive counselling should take place and the individual seeking advice should be given time to consider. The individual seeking advice faces a series of questions regarding the potential implications of a genetic test which not only affect herself but also her environment.
In high-risk situations prophylactic mastectomy is an established surgical measure and intensified surveillance is a conservative approach. The latter includes semi-annual clinical breast examination with ultrasound starting from age 25 as well as an annual MRI mammography which exhibits the highest reliability compared to other imaging methods.
Medical consultation aims to enable a participatory decision-making process for the individual seeking advice. This requires comprehensive information for the individual seeking advice and incorporation of her preferences. Evidence-based decision aids from professional societies can improve the decisions of the individual seeking advice.
References
S3-Leitlinie Früherkennung, Diagnose, Therapie und Nachsorge des Mammakarzinoms. Version 4.3. 2020. AWMF-Registernummer: 032-045OL. (http://www.leitlinienprogramm-onkologie .de/leitlinien/mammakarzinom). search from 03.11.2022
Arbeitsgemeinschaft Gynäkologische Onkologie e. V. Früherkennung und Diagnostik. (https://www.ago-online.de/leitlinien-empfehlungen/leitlinien- empfehlungen/kommission-mamma). search from 03.11.2022
Deutsches Konsortium Familiärer Brust- und Eierstockkrebs. Konsensusempfehlungen des Konsortiums (Stand 2022). (https://www.konsortium-familiaerer- brustkrebs.de/konsensusempfehlung/). search from 03.11.2022
Robert Koch-Institut, Zentrum für Registerdaten. Brust- krebs (Mammakarzinom). (https://www.krebsdaten.de/Krebs/DE/Content/Krebsarten/Brustkrebs/brustkrebs_no de.html#:~:text=Brustkrebs%20(Mammakarzinom)&text=Mit%20zuletzt%20rund%207 1.375%20Neuerkrankungen,Prozent%20aller%20Neuerkrankungen%20betri%EF%AC% 80t%20 M%C3%A4nner.). search from 03.11.2022
Antoniou A et al. Average risks of breast and ovarian cancer associated with BRCA1 or BRCA2 mutations detected in case Series unselected for family history: a combined analysis of 22 studies. Am J Hum Genet 2003; 72: 1117–30
Goldberg JI & Borgen PI. Breast cancer susceptibility testing: past, present and future. Expert Rev Anticancer Ther 2006; 6: 1205–14
Engel C et al. Breast cancer risk in BRCA1/2 mutation carriers and noncarriers under prospective intensified surveillance. Int J Cancer 2020; 146: 999–1009
Fachal L et al. Fine-mapping of 150 breast cancer risk regions identifies 191 likely target genes. Nat Genet 2020; 52: 56–73
Dorling L et al. Breast Cancer Association Consortium. Breast Cancer Risk Genes - Association Analysis in More than 113,000 Women. N Engl J Med 2021; 384: 428–39
Hu C et al. A Population-Based Study of Genes Previously Implicated in Breast Cancer. N Engl J Med 2021; 384: 440–51
Yang X et al. Ovarian and Breast Cancer Risks Associated With Pathogenic Variants in RAD51C and RAD51D. J Natl Cancer Inst 2020; 112: 1242–50
Alm El-Din MA et al. Breast cancer after treatment of Hodgkin‘s lymphoma: risk factors that really matter. Int J Radiat Oncol Biol Phys 2009; 73: 69–74
Preston DL et al. Radiation effects on breast cancer risk: a pooled analysis of eight cohorts. Radiat Res 2002; 158: 220–35
Travis LB et al. Cumulative absolute breast cancer risk for young women treated for Hodgkin lymphoma. J Natl Cancer Inst 2005; 97: 1428–1437.
Tyrer J, Duffy SW, Cuzick J. A breast cancer prediction model incorporating familial and personal risk factors. Stat Med 2004; 23: 1111–30
Ikonopedia. IBIS (International Breast Cancer Intervention Study). Online Tyrer-Cuzick model breast cancer risk evaluation tool – IBIS risk assessment tool v8 .0b. (https://ibis.ikonopedia .com/). search from 03.11.2022
Bundesministerium für Gesundheit. Krebsfrüherkennungsuntersuchung in der gesetzlichen Krankenversicherung (§ 25 Abs. 2 SGB V) /Mammographie. Informationsblatt Nr. 315-02. (https://www.bundesgesundheitsministerium.de/fileadmin/Dateien/3_Downloads/M/ Mammografie/Infoblatt_Krebsfrueherkennung_Mammographie .pdf). search from 03.11.2022
Deutsches Konsortium Familiärer Brust- und Eierstockkrebs. Intensivierte Früherkennung. Früherkennung durch moderne Bildgebung. (https://www.konsortium-familiaerer-brustkrebs .de/betreuungskonzept/praevention/intensivierte-frueherkennung/). search from 03.11.2022
Jakub JW et al. Oncologic Safety of Prophylactic Nipple- Sparing Mastectomy in a Population With BRCA Mutations: A Multi-institutional Study. JAMA Surg 2018; 153: 123–9
Jeffers L et al. Interventions to improve psychosocial well-being in female BRCA- mutation carriers following risk-reducing surgery. Cochrane Database Syst Rev 2019; 10: CD012894
Scheepens JCC et al. Contralateral prophylactic mastectomy: A narrative review of the evidence and acceptability. Breast 2021; 56: 61–9
Bick U et al. German Consortium for Hereditary Breast and Ovarian Cancer (GC-HBOC). High-risk breast cancer surveillance with MRI: 10-year experience from the German consortium for hereditary breast and ovarian cancer. Breast Cancer Res Treat 2019; 175: 217–28
Gödde E. Erbliche Krebsdisposition: Familienplanung zwischen Angst und Verantwortung. EHK 2010; 59: 189–98
Langewitz W. Patientenzentrierte Kommunikation. In: Adler RH, Herzog W, Joraschky P, Köhle K, Langewitz W, Söllner W, Wesiak W, Hrsg. Uexküll, Psychosomatische Medizin. Theoretische Modelle und klinische Praxis. München: Urban & Fischer; 2011. S. 338–47
Downloads
Published
Issue
Section
License
Copyright (c) 2023 Florian Dammann

This work is licensed under a Creative Commons Attribution 4.0 International License.
This license requires that reusers give credit to the creator. It allows reusers to distribute, remix, adapt, and build upon the material in any medium or format, even for commercial purposes.








