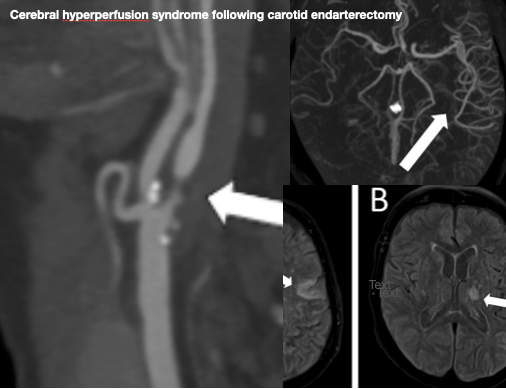
Cerebral hyperperfusion syndrome following carotid endarterectomy
DOI:
https://doi.org/10.59667/sjoranm.v18i1.14Keywords:
cerebral hyperperfusion, carotid endarterectomy, complicationAbstract
Introduction: Cerebral hyperperfusion syndrome (CHS) is a rare but potentially fatal complication following carotid revascularization procedures, particularly carotid endarterectomy (CEA), which is commonly used to treat extracranial carotid stenosis, which is a cause of approximately 15% of all strokes. CHS is characterized by non-ischemic headaches, seizures, and neurological deficits.
Case Report: A 73-year-old woman presented with convulsions three days after undergoing a left CEA for 97% stenosis. Initial symptoms included blurred vision, vertigo, and facial paralysis. Imaging revealed left cerebral hemisphere hypervascularization on CT and vasogenic oedema on MRI, consistent with CHS. Despite clinical deterioration, the patient fully recovered following corticosteroid treatment and was discharged without sequelae.
Discussion: CHS symptoms range from mild headaches to seizures and coma. Although uncommon, the condition carries a high risk of mortality. Pathophysiology involves impaired cerebral autoregulation due to chronic ischemia. Diagnosis relies on imaging, though no standardized criteria exist.
Conclusion: Given its delayed onset and potentially devastating consequences, CHS must be considered in post-CEA or stenting patients. Early recognition and management are essential to prevent adverse outcomes.
References
1. Huibers AE, Westerink J, de Vries EE, et al. Editor’s Choice – Cerebral Hyperperfusion Syndrome After Carotid Artery Stenting: A Systematic Review and Meta-analysis. European Journal of Vascular and Endovascular Surgery. Elsevier Ltd; 2018;56(3):322–333. doi: https://doi.org/10.1016/j.ejvs.2018.05.012
2. Lin YH, Liu HM. Update on cerebral hyperperfusion syndrome. J Neurointerv Surg. 2020;12(8):788–793. doi: https://doi.org/10.1136/neurintsurg-2019-015621
3. Wang GJ, Beck AW, DeMartino RR, Goodney PP, Rockman CB, Fairman RM. Insight into the cerebral hyperperfusion syndrome following carotid endarterectomy from the national Vascular Quality Initiative. J Vasc Surg. Society for Vascular Surgery; 2017;65(2):381-389.e2. doi: https://doi.org/10.1016/j.jvs.2016.07.122
4. Fan X, Zuo Z, Lin T, et al. Arterial transit artifacts on arterial spin labeling MRI can predict cerebral hyperperfusion after carotid endarterectomy: an initial study. Eur Radiol. European Radiology; 2022;32(9):6145–6157. doi: https://doi.org/10.1007/s00330-022-08755-x
Downloads
Published
Issue
Section
License
Copyright (c) 2025 Thomas Saliba, Olivier Cappeliez, Henri Maisonnier, Sanjiva Pather, Ilias Bennouna

This work is licensed under a Creative Commons Attribution 4.0 International License.
This license requires that reusers give credit to the creator. It allows reusers to distribute, remix, adapt, and build upon the material in any medium or format, even for commercial purposes.








